Clinical trials are research studies conducted with human volunteers to evaluate the safety and efficacy of new medical treatments, interventions, or drugs. These trials aim to answer specific questions about potential treatments and contribute to scientific knowledge. They are crucial in advancing medical understanding and improving patient care. Clinical trials follow rigorous protocols and are conducted in phases, each designed to address different aspects, such as safety, dosage, and effectiveness. Patient participation in clinical trials is voluntary and plays a pivotal role in shaping the future of healthcare by helping bring innovative treatments to the forefront.
Patient perspectives are invaluable in shaping medical research, particularly in the realm of clinical trials. Incorporating the views and experiences of individuals participating in these trials is essential for several compelling reasons:
Real-World Relevance:
- Patients provide insights into how a medical intervention or treatment impacts their daily lives.
- Understanding real-world implications helps researchers design interventions that align with patients’ needs.
Enhancing Patient-Centricity:
- Patient-centric research focuses on improving outcomes that matter most to patients.
- By considering patient perspectives, clinical trials can prioritize factors such as quality of life and treatment tolerability.
Informed Decision-Making:
- Patients who are well-informed about the goals and potential benefits/risks of a clinical trial can make more educated decisions about participation.
- Informed consent processes gain significance when they are shaped to meet the understanding and preferences of patients.
Addressing Barriers to Participation:
- Patient perspectives shed light on barriers that may prevent individuals from participating in clinical trials.
- By addressing these barriers, researchers can enhance recruitment and create more diverse and representative study populations.
Optimizing Trial Design:
- Feedback from patients aids in refining trial protocols.
- Patient insights contribute to the development of more patient-friendly trial designs, potentially improving adherence and overall study success.
Promoting Trust and Collaboration:
- A collaborative relationship between researchers and patients fosters trust.
- Patients who feel heard and valued are more likely to engage actively in the research process.
Accelerating Drug Development:
- Patient perspectives can expedite drug development by streamlining research processes.
- Understanding patient priorities helps researchers focus on endpoints that matter most, potentially leading to faster approval and availability of new treatments.
Ethical Considerations:
- Recognizing and respecting patient autonomy is a fundamental ethical principle.
- Incorporating patient perspectives ensures that research aligns with ethical standards and respects individual choices.
Post-Trial Implementation:
- Patient insights extend beyond the trial’s conclusion.
- Understanding patient perspectives aids in planning for the implementation of successful interventions in real-world healthcare settings.
In the intricate web of clinical research, the patient perspective serves as the linchpin, a vital element that can shape the success and impact of a clinical trial. Recognizing and prioritizing the needs, experiences, and concerns of the clinical trials patient is not just ethical; it’s a strategic imperative for organizations like Horizon Trials. Here’s why:
Human-Centric Approach: Clinical trials are fundamentally about people—individuals who are often navigating challenging health conditions. By placing the clinical trials patient at the center of the process, Horizon Trials adopts a human-centric approach. Understanding their fears, expectations, and motivations becomes integral to designing trials that are not only scientifically rigorous but also compassionate and considerate.
Enhancing Patient Recruitment: One of the significant challenges in clinical trials is patient recruitment. Patients may be unaware of trials relevant to their conditions, or they might hesitate due to concerns about the unknown. Horizon Trials, by integrating AI and ML technologies, addresses this challenge directly. By facilitating a more efficient and intelligent patient matching process, the platform enhances the chances of patients finding trials that align with their needs, fostering a smoother recruitment process.
Empowering Informed Decision-Making: Informed consent is a cornerstone of ethical clinical trials. Patients need comprehensive information about the trial, its potential benefits, and associated risks to make informed decisions. Horizon Trials not only connects patients with relevant trials but also provides them with accessible information, empowering them to actively participate in decisions about their healthcare journey.
Reducing Patient Burden: Traditional recruitment methods often involve extensive travel and time commitments, placing a burden on patients already dealing with health challenges. Horizon Trials, by leveraging technology, aims to alleviate this burden. Through features like Mobile Recruitment (MoRe), the platform helps in reducing the travel burden for patients, making participation more feasible and inclusive.
Ensuring Ethical Treatment: Respecting patient rights, safety, and dignity is non-negotiable in clinical trials. Horizon Trials, by protecting user data until explicit consent is provided, maintains a commitment to ethical treatment. This approach not only aligns with regulatory requirements but also fosters trust between patients and the platform.
Contributing to Treatment Innovation: Patients are not passive subjects; they are active contributors to medical advancements. Their participation in clinical trials is a vital link in the chain of medical progress. Horizon Trials recognizes this and, by streamlining the patient matching process, aims to contribute to the innovation of treatments that can positively impact not just individual patients but entire communities.
The clinical trials patient perspective is not just relevant; it is transformative. By recognizing the unique needs of patients, Horizon Trials is not only enhancing the efficiency of clinical trials but also contributing to a paradigm shift where patients are active partners in the advancement of medical science.
The Clinical Trials Landscape
Clinical trials play a pivotal role in advancing medical knowledge and improving patient care. These structured investigations, typically involving human volunteers, are designed to evaluate the safety and efficacy of new medical interventions, including drugs, treatments, and medical devices. Through meticulously planned phases, starting from small-scale studies to large-scale trials, researchers gather essential data to determine the benefits and potential risks of a new intervention. Clinical trials are crucial for gaining regulatory approvals and ensuring that healthcare practices are evidence-based. They contribute significantly to medical breakthroughs, shaping the landscape of treatment protocols and providing innovative solutions for various health conditions. Beyond the scientific realm, clinical trials offer patients an opportunity to access cutting-edge therapies, often when standard treatments have proven ineffective. Moreover, participating in clinical trials is an altruistic contribution to the advancement of medical science, as findings from these trials have far-reaching implications for global health, shaping the future of medicine.
Different phases of clinical trials and their objectives
Clinical trials are conducted in distinct phases, each serving specific objectives to ensure the systematic evaluation of new medical interventions.
Phase I: Safety and Dosage
- Objective: Assess the safety profile and determine the optimal dosage range.
- Participants: Small group of healthy volunteers.
- Focus: Understand how the drug is metabolized and its potential side effects.
Phase II: Efficacy and Side Effects
- Objective: Evaluate the effectiveness of the intervention and further assess safety.
- Participants: Expanded group including patients with the targeted condition.
- Focus: Preliminary data on the intervention’s efficacy and side effect profile.
Phase III: Large-Scale Efficacy
- Objective: Confirm effectiveness, monitor side effects, and compare to existing treatments.
- Participants: Large and diverse patient population.
- Focus: Gather statistically significant data on efficacy and monitor adverse reactions.
Phase IV: Post-Marketing Surveillance
- Objective: Continuously assess long-term risks and benefits after regulatory approval.
- Participants: Population at large, including those with co-existing conditions.
- Focus: Detect rare or long-term side effects and optimize usage in real-world settings.
These phases are critical in establishing the safety, efficacy, and practicality of new interventions, guiding their journey from initial development to widespread use in clinical practice.
Patient participation in clinical trials is of paramount importance, serving as the linchpin for advancements in medical research and the development of novel treatments. It is through the active involvement of patients that researchers gain invaluable insights into the safety, efficacy, and potential side effects of new drugs and therapies. Patients who choose to participate contribute not only to their own health but also to the collective knowledge that propels medical science forward. This involvement is a testament to the altruism and courage of individuals willing to be pioneers in healthcare, often undergoing experimental treatments to pave the way for improved, more effective options in the future. Beyond individual benefits, patient participation is foundational for the generalizability and applicability of research findings, ensuring that medical interventions are relevant and effective across diverse populations. Moreover, it fosters a collaborative partnership between patients and the medical community, emphasizing a patient-centered approach in the development of healthcare solutions. The significance of patient participation extends beyond the confines of a trial, influencing the broader landscape of medicine by shaping treatment standards, enhancing disease understanding, and ultimately contributing to the betterment of global health.
The Patient’s Decision to Participate
Several factors can influence a patient’s decision to participate in a clinical trial:
Potential Benefits: Patients may be motivated by the prospect of gaining access to cutting-edge treatments that could be more effective than existing options, especially if they have exhausted standard treatments.
Altruism: Some individuals are motivated by a desire to contribute to medical research and the development of new therapies that could benefit others, even if they themselves may not directly benefit.
Access to Care: Clinical trials often provide participants with close monitoring by medical professionals, access to leading experts, and comprehensive care, which can be appealing, especially for those with serious or chronic conditions.
Financial Considerations: In some cases, patients may be compensated for their time and expenses related to participation. This can be a factor, especially for individuals facing economic challenges.
Lack of Treatment Alternatives: For individuals with conditions for which standard treatments are not effective, participating in a clinical trial may represent a viable and potentially promising option.
Family or Peer Influence: Recommendations or experiences shared by family members, friends, or peers who have participated in clinical trials can significantly impact an individual’s decision.
Concerns About Standard Treatments: Patients dissatisfied with or skeptical about traditional treatment options may see clinical trials as an avenue to explore alternative or more innovative approaches.
Fear of Placebo: Some patients might be concerned about receiving a placebo instead of an active treatment. Clear communication about the trial design can help manage this concern.
Potential Risks: Patients carefully consider potential risks associated with experimental treatments. Clear communication about the known and unknown risks is crucial for an informed decision.
Impact on Daily Life: The logistics of participating in a trial, including time commitments, travel, and potential impact on daily life, can influence a patient’s decision.
Effective communication and education about the trial, along with addressing any concerns or misconceptions, are essential to ensuring that patients make informed decisions about their participation.
Common misconceptions and concerns about clinical trials
Several common misconceptions and concerns surround clinical trials, often contributing to hesitancy or reluctance among potential participants. It’s crucial to address these to ensure a more informed understanding of clinical trials:
Placebo Misconception: Many individuals fear receiving a placebo instead of active treatment. In reality, placebos are used ethically, and participants are informed if a placebo is part of the study design.
Experimental Treatment Risks: Concerns about the safety of experimental treatments may deter participation. Participants are informed about potential risks, and trials are designed with rigorous safety protocols.
Loss of Control: Some worry about losing control over their health decisions during a trial. Informed consent ensures participants understand the trial and can withdraw at any time.
Fear of Side Effects: Concerns about adverse effects, both known and unknown, are common. Rigorous safety monitoring and informed consent help manage these concerns.
Exclusivity: Some think clinical trials are only for individuals with severe illnesses. Trials cover a wide range of conditions, and some seek healthy volunteers for specific research.
Perceived Ineffectiveness: Individuals may doubt the effectiveness of experimental treatments. Rigorous trial designs aim to demonstrate safety and efficacy before treatments become standard.
Fear of Being a Guinea Pig: Participants may worry about being treated like “guinea pigs.” Ethical guidelines and informed consent prioritize participant welfare and autonomy.
Long-Term Impact: Concerns about long-term effects and impacts on future insurability are common. Legal and ethical safeguards prevent discrimination based on trial participation.
Complexity of Trials: The complexity of trial protocols and medical jargon may be intimidating. Clear communication and education help participants understand the process.
Time Commitment: The perceived time commitment for clinical trial participation can be a barrier. Trial organizers often strive to minimize inconvenience and clearly outline time expectations.
Fear of Randomization: Randomization in clinical trials can be misunderstood. Participants are informed about random assignment, ensuring fairness in treatment allocation.
Lack of Access to Results: Concerns about not receiving information about trial outcomes may arise. Ethical guidelines often require researchers to share results with participants.
Addressing these misconceptions involves transparent communication, comprehensive education, and fostering an environment where potential participants feel heard and respected. Providing accessible information about the clinical trial process is essential for building trust and encouraging informed decision-making.
The Role of Information and Education in Patient Decision-Making
Information and education play pivotal roles in shaping patient decision-making, especially in the context of healthcare choices and participation in clinical trials. Informed decision-making relies on a comprehensive understanding of available options, potential risks, and anticipated benefits. For patients considering participation in clinical trials, access to clear and digestible information about the trial’s purpose, procedures, and potential outcomes is crucial. It enables individuals to weigh the potential risks against the benefits, fostering a sense of autonomy in their healthcare journey. Education about the scientific process behind clinical trials, the significance of randomized control, and the ethical standards governing research contributes to demystifying complex concepts. Through transparent communication and accessible educational resources, patients can navigate the often intricate landscape of medical research, empowering them to make decisions aligned with their values and health goals. Furthermore, a well-informed patient is more likely to actively engage in discussions with healthcare professionals, fostering a collaborative and patient-centered approach to healthcare decision-making. In essence, information and education become empowering tools, enabling patients to navigate the complexities of healthcare choices and make decisions aligned with their preferences, ultimately contributing to better health outcomes and a more patient-centric healthcare system.
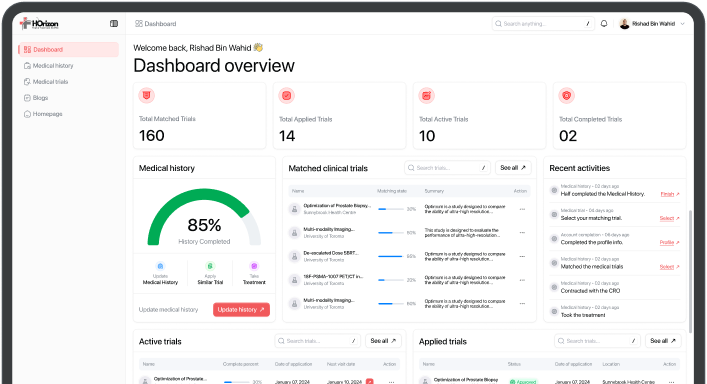
Horizon Trial: A Closer Look
Horizon Trials emerged as a pioneering force in the realm of clinical trial facilitation, harnessing the power of cutting-edge technologies to revolutionize patient recruitment and trial matching processes. What sets Horizon Trials apart is its innovative use of Artificial Intelligence (AI) and Machine Learning (ML) technologies, bringing a new level of efficiency and precision to the identification and vetting of patients for specific clinical studies conducted by Contract Research Organizations (CROs). This platform not only caters to the needs of CROs by streamlining their participant selection process but also prioritizes the patient experience by providing a user-friendly interface to explore available treatments and clinical trials. Unlike traditional methods, Horizon Trials mitigates the need for in-person vetting during the early stages of participant selection, significantly reducing costs and time for CROs. The platform’s agility and commitment to leveraging emerging technologies position it as a trailblazer in the industry, offering a sophisticated solution to the challenges of patient recruitment and clinical trial matching. Horizon Trials stands as a beacon at the intersection of healthcare and technology, with a mission to enhance the efficiency, accessibility, and success rates of clinical trials, ultimately contributing to advancements in medical research and improved patient outcomes.
Impact on Patient Health
Participation in clinical trials presents both potential benefits and risks for patients. On the positive side, patients in clinical trials gain access to cutting-edge treatments and therapies that might not be available through standard care. This early access can be particularly crucial for individuals with serious or rare conditions for whom conventional treatments have proven ineffective. Clinical trial participants often receive close medical supervision and monitoring, ensuring that any emerging issues are promptly addressed. Moreover, contributing to medical research can be personally fulfilling for patients, as they play a role in advancing scientific knowledge and potentially improving treatments for future generations. However, there are inherent risks involved, such as the uncertainty of the treatment’s effectiveness and potential side effects that may not be fully understood. The experimental nature of clinical trials means that outcomes are unpredictable, and there is a possibility that the treatment might not be as effective as anticipated. Patients also need to consider the time commitment and potential inconvenience associated with the frequent medical visits and procedures typical in clinical trials. Informed consent, a critical aspect of ethical clinical research, ensures that patients are aware of both the potential benefits and risks before deciding to participate, promoting transparency and patient autonomy in the decision-making process.
The Role of Clinical Trials in Advancing Treatment Options
Clinical trials play a pivotal role in advancing treatment options, driving medical progress, and enhancing patient care. These structured and rigorous studies are designed to evaluate the safety and efficacy of new treatments, therapies, or interventions before they are made widely available. Through carefully conducted phases, clinical trials help researchers understand how a potential treatment interacts with the human body, its side effects, and its overall impact on health.
These trials are not limited to testing new drugs; they encompass a wide range of medical interventions, including surgical procedures, medical devices, behavioral therapies, and preventive strategies. Clinical trials contribute significantly to scientific knowledge, enabling healthcare professionals to make evidence-based decisions about the best course of treatment for various conditions.
Participation in clinical trials is crucial for patients, as it provides access to innovative treatments that may be more effective than existing options. By involving diverse populations in these studies, researchers can better understand how different groups respond to treatments, ensuring that medical advancements are applicable to a broad range of individuals.
Moreover, clinical trials often serve as the foundation for breakthroughs in medical science, leading to the development of new standards of care. They are essential for gaining regulatory approval for new treatments and are a key driver of innovation in the healthcare industry. Overall, the role of clinical trials is indispensable in advancing treatment options, improving patient outcomes, and pushing the boundaries of medical knowledge.
Patient-Centric Approaches
The landscape of clinical trials has undergone a significant evolution towards more patient-centric models, reflecting a fundamental shift in the approach to medical research and healthcare. Traditionally, clinical trials were structured around a model where researchers held primary control, focusing on meeting regulatory requirements and scientific objectives. However, recognizing the importance of the patient’s perspective, recent years have witnessed a paradigm shift toward a more patient-centric approach.
In this modern approach, the emphasis is not only on assessing the safety and efficacy of treatments but also on addressing the unique needs, preferences, and experiences of patients. Patient-centric clinical trials prioritize involving patients in the design, planning, and execution phases. This includes incorporating patient input in determining research priorities, selecting relevant outcomes, and even designing trial protocols.
Several factors have contributed to this transformation. Increased awareness and advocacy for patient rights and involvement, advancements in technology allowing for remote monitoring and virtual trials, and a growing recognition of the value of patient-reported outcomes have all played crucial roles.
Patient-centric clinical trials aim to enhance the overall trial experience for participants by reducing burdensome procedures, improving communication, and fostering a more collaborative relationship between researchers and patients. This approach not only enhances recruitment and retention rates but also produces more relevant and meaningful results.
The adoption of patient-centric models aligns with the broader trend of personalized medicine, recognizing that individuals respond differently to treatments based on their unique characteristics. This evolution reflects a commitment to ensuring that clinical trials are not only scientifically rigorous but also respectful of the individuals who participate, ultimately contributing to more effective and patient-friendly healthcare solutions.
The Future of Clinical Trials
Clinical trial design is experiencing a transformative shift with a growing emphasis on patient-centricity. One of the emerging trends is the integration of patient perspectives in the early stages of trial planning. This involves incorporating patient input in the selection of meaningful endpoints, trial protocols, and even the design of informed consent processes. Additionally, there’s a move towards more decentralized and hybrid trial models, leveraging technologies that enable remote monitoring, reducing the need for frequent site visits, and making participation more convenient for patients.
Technological Advancements Enhancing Patient Experience
Technological advancements are playing a pivotal role in enhancing the overall patient experience in clinical trials. Mobile health applications, wearable devices, and telehealth platforms are being increasingly utilized. These innovations not only facilitate real-time data collection but also empower patients by providing them with tools to actively engage in their healthcare. Wearables, for instance, can monitor vital signs, adherence to medications, and lifestyle factors, offering a more comprehensive and continuous picture of a patient’s health, thereby contributing to more precise and personalized interventions.
Potential Breakthroughs and Their Impact on Patient Perceptions
Anticipated breakthroughs in medical research and drug development are influencing how patients perceive and engage with clinical trials. Advancements in areas like gene therapies, immunotherapy, and precision medicine offer new hope for conditions that were previously considered untreatable. The promise of more targeted and effective treatments is changing patient perceptions about the risks and benefits of participating in clinical trials. Additionally, breakthroughs in data analytics and artificial intelligence are improving the efficiency of trials, potentially reducing the duration and resource requirements, making participation in trials more appealing to patients.
These trends collectively contribute to a more patient-friendly landscape in clinical trials, fostering increased participation, better retention, and ultimately, a healthcare system that is more aligned with the needs and expectations of the individuals it serves.
In conclusion, patients play a really big role in making new medicines and treatments. The things they say and do in clinical trials help scientists understand what works and what doesn’t. This is super important for making better and safer medicines. When patients take part, it helps everyone. It’s like being a hero in the story of finding new cures and treatments. So, it’s really good when patients and scientists talk a lot and understand each other. If we all share our thoughts and ideas, we can make medicine better for everyone. Let’s keep talking and working together to make sure everyone gets the best care.